Welcome to pregnancy week 28! You’ve made it to the third and final trimester! You’ll have your new bundle of joy in your arms before you know it!
How your baby is growing during pregnancy at week 28
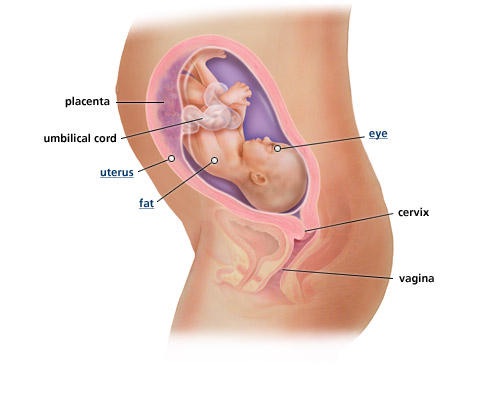
Your growing baby is now about the size of a large eggplant, or about 2 1/4 pounds and is just over 14 inches in length. She has developed eyelashes now and practices blinking. Baby will turn her head toward any bright light shown into the womb. Her eyes will have likely turned a bluish color if she is Caucasian, and a darker brown or gray color for babies of African-American, Hispanic, or Asian decent.
Your baby’s lungs are now developed enough that if she were to be born today, there is a great chance of survival! This is great news! Still, it is absolutely in baby’s best interest to stay in the womb until as late as 40-42 weeks.
She is also packing on the pounds in preparation for life outside the womb, which means her wrinkly skin will start to smooth out. Your baby is settling herself into her birthing position, with her head snugly tucked downward into your pelvis. She also is practicing hiccuping, swallowing (amniotic fluid), sucking, and coughing! Baby is working out her own sleep cycle now as well, including, some say, REM sleep, or the cycle of sleep in which humans dream. Only a little while longer before baby is ready to meet you!
Photo credit: https://www.babycenter.com/fetal-development-images-28-weeks
How your body is changing
If you haven’t already experienced it, sciatic pain could be coming your way this week. This is a tingle that ranges from annoying to extremely painful that radiates down your hips and legs from your lower back. Try a heating pad, or think about scheduling an appointment with a chiropractor.
With baby working out her sleep cycle, you may not be getting great sleep yourself, with all of her exercising in the middle of the night. It’s normal to worry about whether or not your baby is active enough. Generally speaking, it’s good to feel about ten movements from your baby inside of an hour’s time. If her movements are significantly less often than this, be sure to tell your practitioner. Some babies just aren’t as active, so you’ll settle into knowing what is normal for your own little one.
Restless leg syndrome is a common pregnancy ailment during week 28 pregnancy. This is the tingly, or “creepy-crawly” feeling in your lower extremities. Often women with RLS describe a feeling that they can’t stop moving their legs. This feeling can be especially intense in the evening hours. While it’s not understood what causes RLS, caffeine may intensify symptoms, so if you’re suffering, try limiting your caffeine intake, stretching, and massaging your legs. For most women, RLS goes away upon delivering your baby.
Your doctor will likely want to see you twice per month at this stage (changing to once per week for your final month of pregnancy). He will likely test your urine, and measure your belly and weight, as usual, but could also soon begin blood tests for significant STD’s and anything else that you or your baby may be at risk for.
Things to do during pregnancy week 28
It’s a good idea to start thinking about who your baby’s pediatrician will be. Typically your baby be seen by a doctor during the first few days of birth. Many expectant mothers feel best if they can see the same doctor from the very beginning. Get recommendations for great doctors in your area from trusted friends and family with children. And while you’re thinking about it, you and your partner should make a decision about circumcision if your baby is a boy. Opinions about circumcision vary, so do some research and make an informed decision you feel would be best for your baby.
Cord blood banking is a service many families choose. You should talk to your doctor about your options. Mothers who choose cord blood banking store blood from the baby’s umbilical cord right after delivery. They then pay a facility to safely store the collected blood to be used in a situation where the baby could benefit from its use in cases of blood and immune diseases.
If you haven’t already done so, it’s also a great time to schedule childbirth classes. Many popular classes fill up quickly and require advanced notice to be admitted. Your doctor may be able to recommend a breastfeeding class as well. Be sure to check your insurance to see if the cost of your classes could be covered! It is completely normal to feel some anxiety about labor and delivery, especially if this is your first child! It is helpful to do your research about what to expect. Reading positive birth stories from other women can be encouraging and calming.
Featured photo credit: January 2013/Phaling Ooi via flickr.com